The advent of anti-vascular endothelial growth factors (anti VEGF) agents has revolutionised treatment for a number of ocular conditions including age related macular degeneration and cystoid macula oedema from diabetic maculopathy and retinal vein occlusions. Mr Jasani offers a detailed initial and follow up assessments, relevant investigation using state of the art imaging systems, and comprehensive treatment with retinal lasers and intravitreal injections for the above conditions.
Age Related Macular Degeneration (ARMD)
ARMD as its name suggests is a degenerative condition affecting the central part of the retina called the macula (which is responsible for your fine detailed central vision). The macula degenerates with loss of crucial cells that help you see the fine details of your vision and thus affecting things like reading, watching television, driving or even recognising faces. It is the commonest cause of visual impairment in the Western world. We do not know the exact cause for ARMD but factors such as age, previous history of smoking, poor diet and also genetics have shown to be associated with it. There are 2 main types of ARMD; dry and wet and both are interchangeable.
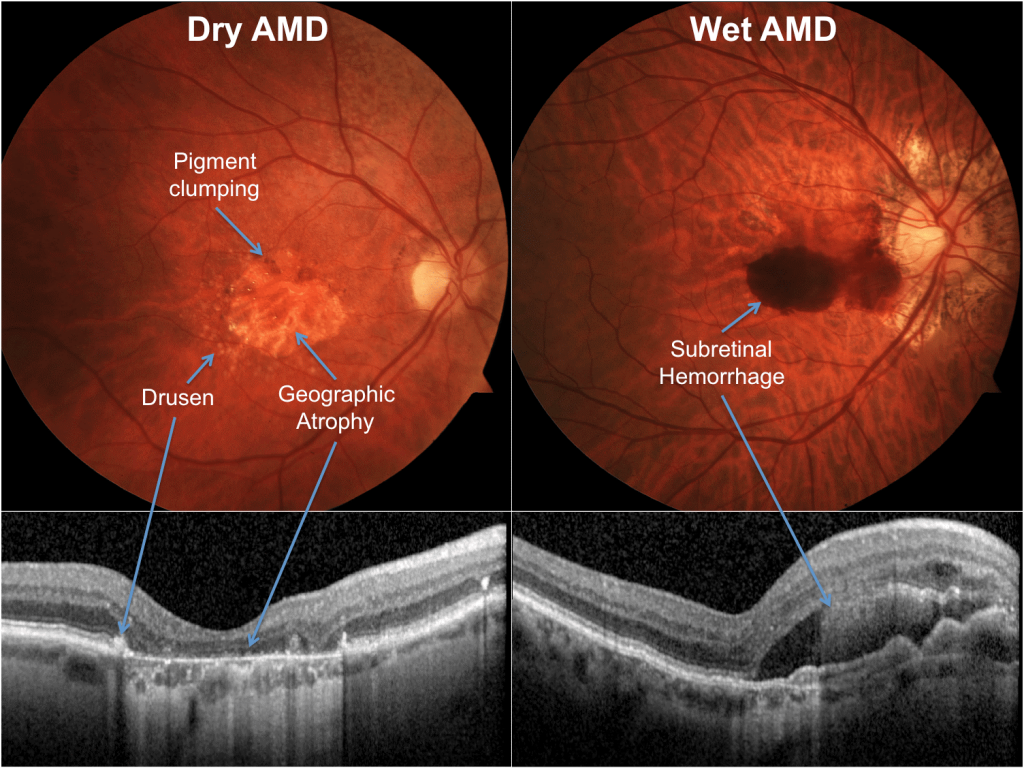
Dry ARMD
accounts for almost 90% of patients with ARMD and develops more slowly compared to the wet subtype. It has no approved treatment to date although gene therapy trials have started around the world. Patients with dry ARMD are not regularly followed up in the NHS. However, patients should be warned to present themselves to a retinal specialist if they notice sudden worsening in vision or new onset distortion as it could be a sign of wet ARMD.
Wet ARMD
accounts for approximately 10% of patients and has a much faster progression rate than the dry ARMD subtype. It can have drastic devastating effects on patients vision mainly due to leakage from ‘new blood vessels’ underneath the retina. These blood vessels bleed relatively easily damaging the overlying retina, displacing it and ultimately scarring it with corresponding loss in vision. The last decade has seen a transformation in the treatment of wet ARMD with the advent of anti VEGF injections. These therapies include Avastin (Bevacizumab), Lucentis (Ranibizumab) and Eylea (Aflibercept) have shown to not only stabilise vision but also improve it in certain patients. They are initially given every month for 3 months then tailored individually depending on the response to treatment.
DIABETIC MACULA OEDEMA (DMO)
DMO is the most common cause of sight loss in diabetics. Oedema means fluid retention. When leaky vessels cause fluid to build up in the macula (the central area of your retina responsible for fine central vision), it is known as diabetic macular oedema. It is a complication of diabetic retinopathy and results in a condition very similar to wet AMD. Mr Jasani offers a thorough initial assessment and subsequent follow up, alongside comprehensive management of your diabetic retinopathy, tailoring care to your needs and in-line with latest evidence and research.
People with diabetes are at particular risk of damage to their eyesight. The longer you have diabetes, the greater your chance of developing sight loss. About 90% of people with type 1 diabetes will have some degree of retinopathy after 10 years. For people with type 2 diabetes, the chance of developing retinopathy after 10 years is between 67 and 80%.
In the early stages of diabetes, you may not notice any effect on your vision. If damage causes only microaneurysms (small abnormal dilatation in the blood vessels of the retina), your eyesight can remain good. However, when the blood vessels in or near the macula become damaged, or there is a sudden bleed or leak into the macula, your sight can worsen dramatically. If you notice a sudden change in your vision, you should see your ophthalmologist/retinal specialist as soon as you can.
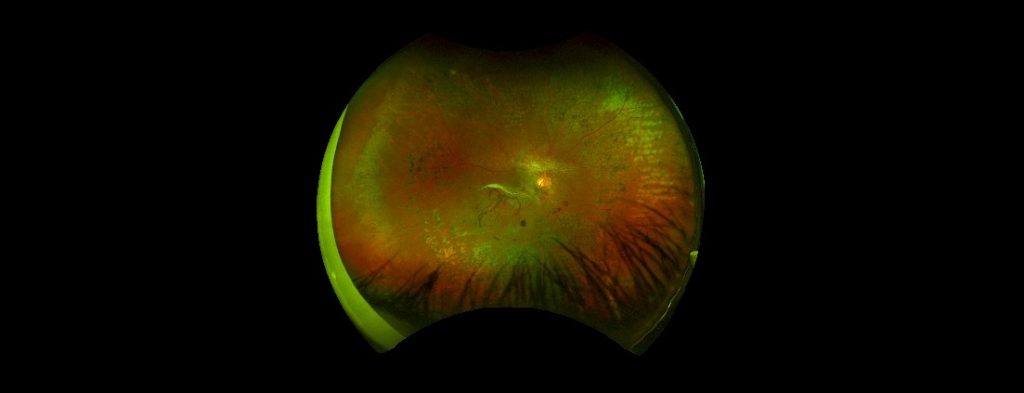
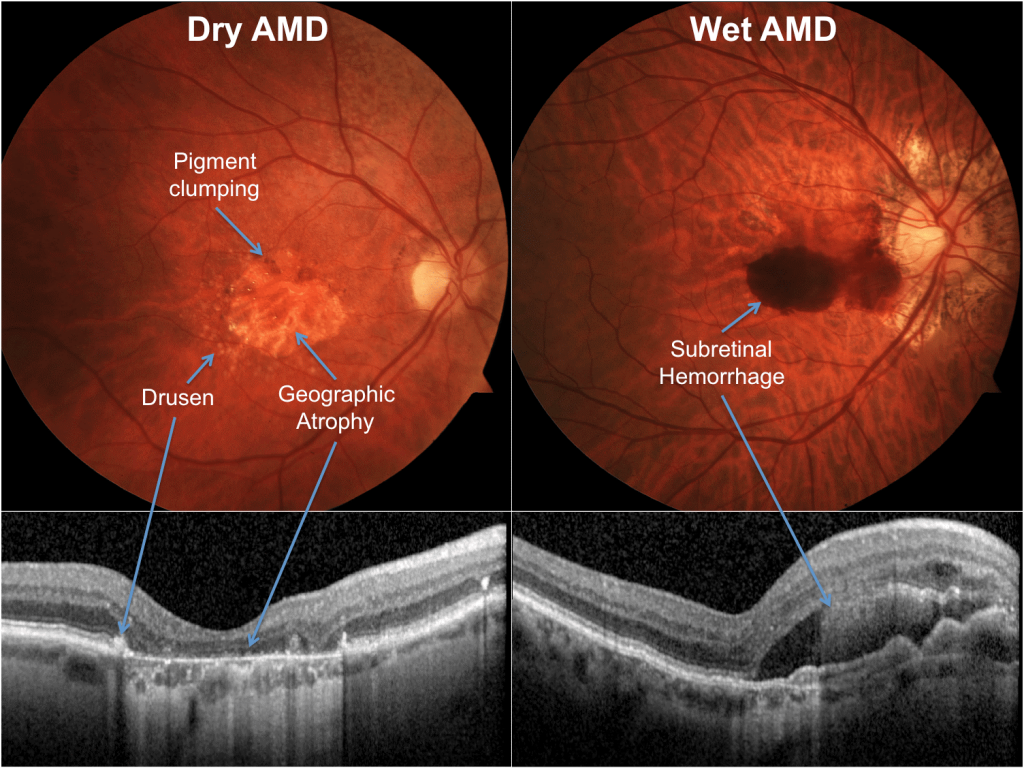
Figure: A widefield picture of the retina showing severe changes due to diabetic retinopathy in a young patient.
DMO can be treated if it is caught early. Although treatments cannot restore sight if there is already significant damage to the macula, they can slow the rate of damage and preserve more of your sight for longer.
Anti-VEGF drugs are injected into the eye to stop fluid leaking from the blood vessels. You will usually have a number of injections in the first few months, then more if later check-ups suggest they are needed.
Some people, including those who have had cataract surgery, may be offered a steroid injection instead. A tiny implant is injected into the eye to gradually release the steroid over several months.
If your DMO doesn’t involve the centre of the macula, you may be offered laser treatment. This usually requires one or more visits to an outpatient laser clinic for treatment by an ophthalmologist.
Figure: OCT images (a scan which shows the layers of the retina in a cross section) taken from a patient with diabetic macula oedema in both eyes (A and B) and following treatment with intravitreal anti VEGF therapy (C and D).
RETINAL VEIN OCCLUSIONS
Retinal vein occlusions are a common cause of sudden, painless reduction or loss in vision particularly in people aged over 60 years. It occurs when an artery presses on and blocks one of the veins in the retina. The blockage of a vein causes blood and other fluids to leak into the retina, which causes damage that reduces vision.

There are 2 types of vein occlusions:
- Branch retinal vein occlusion (BRVO) which results from blockage of any of the four retinal veins (which drain blood from one quadrant of the retina)
- Central retinal vein occlusion (CRVO) which results from obstruction in the main retinal vein with generally more severe consequences.
It is more likely to happen in patients with high blood pressure, high cholesterol, history of smoking, glaucoma and in certain blood disorders.
Treatment include anti-VEGF injections (primarily Eylea, Lucentis) or steroid implants (Ozurdex) injected into the eye is used to treat RVO. The injections have to be repeated over a period of time to work effectively.
Injection treatment aims to stabilise or improve vision. About 45-55% of patients treated with anti-VEGF injections experience a significant gain in vision. Steroid implants achieve a significant gain in vision in up to 30% of patients. 20-30% of patients experience no improvement in vision treatment.
Observation or monitoring is an option for people who prefer not to have treatment for macular oedema. Branch retinal vein occlusions have a better chance of natural resolution than central retinal vein occlusions. However, treatment has been shown to achieve the best results.
