How does Diabetes affect your eyes?
The retina is the light-sensitive layer of cells at the back of the eye that converts light into electrical signals. The signals are sent to the brain which turns them into the images you see.
The retina needs a constant supply of blood, which it receives through a network of tiny blood vessels. Over time, a persistently high blood sugar level can damage these blood vessels in 3 main stages:
- background retinopathy – tiny bulges develop in the blood vessels, which may bleed slightly but don’t usually affect your vision
- pre-proliferative retinopathy – more severe and widespread changes affect the blood vessels, including more significant bleeding into the eye
- proliferative retinopathy – scar tissue and new blood vessels, which are weak and bleed easily, develop on the retina, this can result in some loss of vision
However, if a problem with your eyes is picked up early, lifestyle changes and/or treatment can stop it getting worse.
Diabetes may cause damage to the delicate blood vessels in the central part of the retinal camera film in the eye (macula), producing leakage of fluid and swelling (oedema) resulting in reduced central vision. Untreated, you will probably end up with permanently impaired reading and distance vision and also likely lose your ability to drive. Treatments for DMO are however better than ever, and include laser treatment and intravitreal eye injections (see section under Intravitreal Injections)
Non-proliferative (background) diabetic retinopathy. This is where progressive injury to and blockage of the blood vessels in the more peripheral parts of your retina result in damage to the delicate retinal cells. Your sight will generally not be affected, but you must attend regular screening to monitor progression.
Proliferative Diabetic Retinopathy (PDR)
If the damage to the retina from the blocked blood vessels progresses and becomes significant, it can stimulate the growth of new abnormal, fragile blood vessels from the surface of the retina.
Vitreous Haemorrhage
Left untreated, the abnormal blood vessels can bleed (haemorrhage) into the clear jelly (vitreous humour) which fills most of your eye. This is called a vitreous haemorrhage. Most bleeds are small and clear spontaneously over weeks or months. With small bleeds you will notice sudden worsening of floaters, often with a red tint to them. If, however, your bleed is severe, then you will suffer from severe loss of vision as light will not be able to reach the retina because it is obscured by the vitreous haemorrhage.
Retinal Detachment
If the PDR does not receive sufficient treatment in time, then your condition may worsen to the point where scar tissue may grow on the surface of your retina and contract, causing your retina to detach. This requires surgery which may be needed urgently in some instances. Untreated, there is a very high chance of blindness.
Although modern treatments are very successful in preventing blindness in most people, occasionally poor control and compliance, combined with late presentation and severe disease may result in very high, difficult to control pressures in the eye and total blindness in that eye.

Figure: Colour photograph of the left eye showing proliferative diabetic retinopathy with new vessel growth, bleeding above the retina alongside scar tissue formation causing traction on the retina.
What are the symptoms of diabetic retinopathy?
You won’t usually notice diabetic retinopathy in the early stages, as it doesn’t tend to have any obvious symptoms until it’s more advanced.
However, early signs of the condition can be picked up by taking photographs of the eyes during diabetic eye screening.
Contact your GP or diabetes care team immediately if you experience:
- gradually worsening vision
- sudden vision loss
- shapes floating in your field of vision (floaters)
- blurred or patchy vision
- eye pain or redness
These symptoms don’t necessarily mean you have diabetic retinopathy, but it’s important to get them checked out. Don’t wait until your next screening appointment.

Figure: This colour image shows pre-proliferative diabetic retinopathy with dot and blot haemorrhages, abnormal microvasculature and cotton-wool spots
Is there any treatment for advanced diabetic retinopathy?
For diabetic retinopathy that is threatening or affecting your sight, the main treatments are:
- Laser treatment – to treat the growth of new blood vessels at the back of the eye (retina) in cases of proliferative diabetic retinopathy, and to stabilise some cases of maculopathy
- Intravitreal eye injections – to treat severe maculopathy that’s threatening your sight
- Eye surgery – to remove blood or scar tissue from the eye if laser treatment isn’t possible because retinopathy is too advanced
Laser treatment
Laser treatment is used to treat new blood vessels at the back of the eyes in the advanced stages of diabetic retinopathy. This is done because the new blood vessels tend to be very weak and often cause bleeding into the eye.
Treatment can help stabilise the changes in your eyes caused by your diabetes and stop your vision getting any worse, although it won’t usually improve your sight.
Laser treatment:
- involves shining a laser into your eyes – you’ll be given local anaesthetic drops to numb your eyes; eye drops are used to widen your pupils and special contact lenses are used to hold your eyelids open and focus the laser onto your retina
- normally takes around 20-40 minutes
- is usually carried out on an outpatient basis, which means you won’t need to stay in hospital overnight
- may require more than one visit to a laser treatment clinic
- isn’t usually painful, although you may feel a sharp pricking sensation when certain areas of your eye are being treated
Side effects
After treatment, you may have some side effects for a few hours. These can include:
- blurred vision – you won’t be able to drive until this passes, so you’ll need to arrange for a friend or relative to drive you home, or take public transport
- increased sensitivity to light – it might help to wear sunglasses until your eyes have adjusted
- aching or discomfort – over-the-counter painkillers, such as paracetamol, should help
Possible complications
You should be told about the risks of treatment in advance. Potential complications include:
- reduced night or peripheral (side) vision – some people may have to stop driving as a result of this
- bleeding into the eye or objects floating in your vision (floaters)
- being able to “see” the pattern made by the laser on the back of your eye for a few months
- a small, but permanent, blind spot close to the centre of your vision
Get medical advice if you notice that your sight gets worse after treatment.
Eye injections
In some cases of diabetic maculopathy, injections of a medicine called anti-VEGF may be given directly into your eyes to prevent new blood vessels forming at the back of the eyes.
The main medicines used are called ranibizumab (Lucentis) and aflibercept (Eylea). These can help stop the problems in your eyes getting worse, and may also lead to an improvement in your vision.
During treatment:
- the skin around your eyes will be cleaned and covered with a sheet
- small clips will be used to keep your eyes open
- you’ll be given local anaesthetic drops to numb your eyes
- a very fine needle is carefully guided into your eyeball and the medication is injected
The injections are usually given once a month to begin with. Once your vision starts to stabilise, they’ll be stopped or given less frequently.
Injections of steroid medication may sometimes be given instead of anti-VEGF injections, or if the anti-VEGF injections don’t help.
Risks and side effects of Intravitreal injections
Possible risks and side effects of anti-VEGF injections include:
- eye irritation or discomfort
- bleeding inside the eye
- floaters or a feeling of having something in your eye
- watery or dry, itchy eyes
There’s also a risk that the injections could cause blood clots to form, which could lead to a heart attack or stroke. This risk is small, but it should be discussed with you before you give your consent to treatment.
The main risk with steroid injections is increased pressure inside the eye.
Eye surgery
Surgery may be carried out to remove some of the vitreous humour from the eye. This is the transparent, jelly-like substance that fills the space behind the lens of the eye.
The operation, known as vitreoretinal surgery, may be needed if:
- a large amount of blood has collected in your eye
- there’s extensive scar tissue that’s likely to cause, or has already caused, retinal detachment
During the procedure, the surgeon will make a small incision in your eye before removing some of the vitreous humour, removing any scar tissue and using a laser to prevent a further deterioration in your vision.
Vitreoretinal surgery is usually carried out under local anaesthetic and sedation. This means you will not experience any pain or have any awareness of the surgery being performed.
After the procedure
You should be able to go home on the same day or the day after your surgery.
For the first few days, you may need to wear a patch over your eye. This is because activities such as reading and watching television can quickly tire your eye to begin with.
You will probably have blurred vision after the operation. This should improve gradually, although it may take several months for your vision to fully return to normal.
Your surgeon will advise you about any activities you should avoid during your recovery.
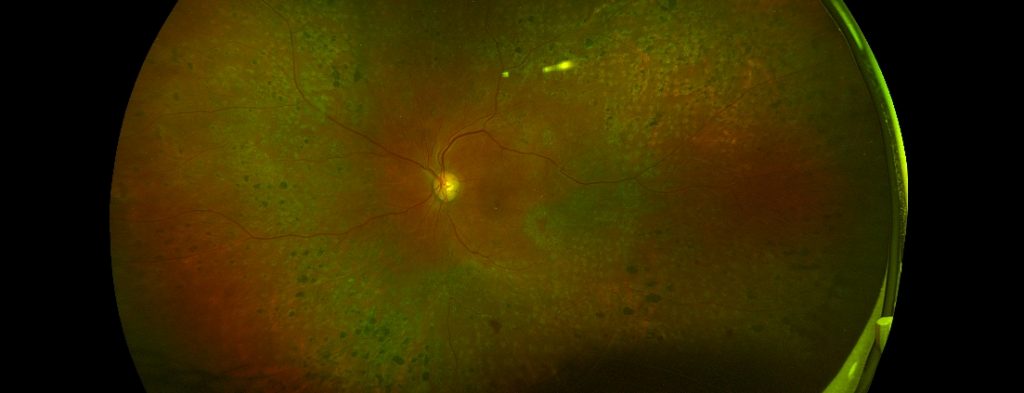
Before: A widefield image of an eye with diabetic retinopathy which has been treated with peripheral laser (PRP) treatment and has now stabilized.
After: The widefield image on the left shows severe tractional retinal detachment from diabetic retinopathy and its appearance after successful surgery. In this case, the patients vision improved significantly and his retinopathy has now stabilized.
